Therapeutic relationships: what a bloody complicated subject.
These relationships are unlike any other – there is a natural power-imbalance and a one-way exchange of information/knowledge about the people involved. This means that those on the professional end of therapeutic relationships, especially with vulnerable patients, are left with the immensely difficult task of working out how best to balance the relationship to aid their patient’s health and wellbeing. Mistakes can be catastrophic and misuse/abuse of the relationship can cause immense damage.
For me, as a ‘particularly complex’ mental health patient with a mixed personality disorder (this means a diagnosis of multiple personality disorders, which boils down to long-standing, deep-seated and severe mental health issues) as well as other mental health problems, with roots of these illnesses stemming from core issues with relationships before I could even comprehend them, I am one of those people for whom therapeutic relationships become especially complicated and important to my care.
Until moving back home in October 2015 after my first contact with mental health services – a long, distressing inpatient stay at a psychiatric hospital – I didn’t really have a concept of a true therapeutic relationship. Then along came my first ever care coordinator and I was fortunate enough that her skills, empathy, patience, persistence, kindness and belief in me allowed us to develop a strong therapeutic relationship at a point where I was determined never to even speak to a mental health professional again. I have recently discovered in an extensive psychotherapy assessment that this was the first time I had ever allowed myself to drop down the extensive guard that I had put up my entire life to protect everyone else from the ‘badness’ that I perceived to be inside of me; this was also the first time that I had ever trusted that someone wouldn’t leave me at the drop of a hat whilst I needed them (obviously excepting personal circumstances or anything unexpected). For the first time ever I had someone who I could be honest with, who I didn’t have to protect from me, who believed in me, who held my hope for me, who would advocate for me, and who I didn’t fear would suddenly leave me for no reason – and all of this held securely in a therapeutic relationship with excellent boundaries.
Then, in November 2016, I found myself in intensive care following a serious suicide attempt, coming round to find that my care coordinator had been removed from me with no contact allowed whilst I was still on the cusp of death and whilst she wasn’t at work. The explanation I was initially given for this was that the team had decided that the severity of my illness and distress was causing harm to my care coordinator, an experienced community psychiatric nurse: my absolute worst fears had come true: I had let down that protective barrier a little and caused harm to a very experienced mental health professional…it must be reality that I am filled with such toxic darkness that if I dare be honest about my thoughts/feelings/needs and accept help then I will hurt others. For the first time in my life I had, with my care coordinator’s skills and help, fought against these life long beliefs/fears to test out a different way of relating to someone in what was supposed to be a safe therapeutic relationship and I had managed to hurt someone, and someone who had the training and support that should have mitigated such a scenario occurring; especially as boundaries were maintained well within the therapeutic relationship. My next care coordinator turned out to be the person who made the decision and she reinforced these beliefs in me. Others did step in and say that actually the decision had nothing to do with my first care coordinator and that it definitely was not because I had impacted her in anyway, that actually it was made as a clinical decision in my best interests, and that I had been given a completely wrong explanation; but the damage was done – the monster within my brain, driven by mental illness and especially personality disorders, had been given solid evidence to back up what it had been telling me all these years, and now there was no fighting it; because of this it was decided that there was no chance of a therapeutic relationship with this care coordinator. The next/current CC decided from the outset to take control, break trust/confidentiality (until I made sure the legal department was consulted, and it was decided that doing so was illegal), repeatedly infer I’m just not trying and take on what feels like a very blaming/shaming attitude towards me. The monster is now so immense and terrifying.
Since the events of November, my mental health and self destructive behaviour (which, for me, is driven by the need to punish myself, increased greatly by guilt/shame, and builds to active suicidality as a need to get rid of the toxicity that is me from the world for the benefit of both everyone else and myself) has spiralled out of a control. Obviously, the connection to the events of November hadn’t escaped me, but it wasn’t until bumping into my first care coordinator (who confirmed to me that in no way did I have any negative impact on her and that she had been informed that the decision to remove her from my care with no contact was a clinical one in my best interests, nothing to do with her) this week, the subsequent meltdown, and that this all coincided with part of my extensive psychotherapy assessment that I realised the core issues within me this had triggered, and that it actually made sense why these events had had the impact that they had. From afar, it must seem bizarre that such a seemingly small event surrounding a professional/therapeutic relationship could cause the deterioration and seemingly irreversible damage that it did.
But, to me, since November it has become undeniable truth that I am toxic to the core and that I must protect everyone from this.
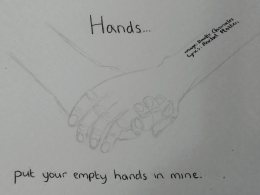
I haven’t been able to form a solid therapeutic relationship with subsequent care coordinators and I have withdrawn further from my personal relationships, and I am left feeling like it is unfair of me to allow myself relationships of any form – why should I risk hurting anyone else? This has left me without that advocate, that person to hold my hope when I can’t, that person who will fight for me, that person who believes and understands me, that person to drive my care in a way that helps me to stay safe and recover.
This may sound like I’m moaning but I promise I am not: I know that I was very lucky with my first care coordinator, and I blame myself for all that has happened since, and I am filled with immense guilt and shame about it all.
I am consumed by fear and self-hatred. I am alone and terrified. I am confused and conflicted.
I am toxic.
I really get how u feel. I wasn’t allowed into a recent meeting about my care because they didntwant me to hear how I ‘made people feel’. Both my long term care coordinator and therapist have been immediately removed with no chance to say goodbye. I too feel poisonous and toxic. How do people making these decisions fail to see the impact it will have on the SU
LikeLiked by 1 person
I’m so, so sorry to hear this and sending lots of love xx
LikeLike